The discussion on the introduction of electronic health records (EHRs) in Germany is in full swing. The Bertelsmann Stiftung aims to add impetus to this debate with an expert report by Professor Peter Haas. Of particular importance here is the conceptual idea of the EHR as a basis for comprehensive treatment management platforms. These EHRs will serve both as a common instrument of service providers and patients, as well as a central instrumental foundation – a hub – for digital process innovation in the healthcare sector. In introducing these records, this mission should be pursued from the very outset.
When talk turns to the topic of patient records, almost everyone has a story to tell: Laboratory results that patients themselves later have to take from the specialist to the family doctor; lost MRT images; or the incomprehensible physician’s letter pressed into patients’ hands when being discharged. Personal anecdotes aside, it is widely recognized that the faults of German healthcare system lie mainly in the interfaces between the various stakeholders and sectors, and that the system is fragmented and information doesn’t flow as it should. So, what would it be like if every (willing) patient had an electronic health record in which all treatment-relevant information was available at any time – a record that all authorized treatment providers and the patient could access? And what would it be like if this record also formed the core of a patient’s entire treatment management, and made the patient an active part of the treatment Team?
The discussion on the national introduction of electronic health records in Germany has (re)gained momentum since the E-Health Act, if not before. In a broad spectrum of projects – such as in the context of innovation funds or the activities of major hospitals – overarching record systems are now emerging, with stakeholders pursing, in part, differing goals and strategies. Against this backdrop, last year, we commissioned an expert report on this topic from Professor Peter Haas, a medical information scientist at the Dortmund University of Applied Science and Arts (Fachhochschule Dortmund) and long-standing spokesperson for the Advisory Council for the Society for Telematics Applications (Gesellschaft für Telematik, gematik). We asked him what needs to happen for electronic health records to gain acceptance in Germany, and how this can serve as a tool for greater patient sovereignty.
This has given rise to an extensive treatise, which examines on 288 pages the most diverse aspects of the topic, including the functional requirements, questions of physical distribution of data, the content strategy, questions of data protection and ethics, informational self-determination, as well as specific recommendations relating to the approach to implementation and governance structure. The result – summarized at a high level: The introduction of electronic health records with high social utility requires a long-term strategy, effective governance, and – with the competitive development of record systems – the expeditious introduction of a binding framework that patients can rely on.
Underlying concept: Electronic health records as an instrumental foundation for digital Transformation
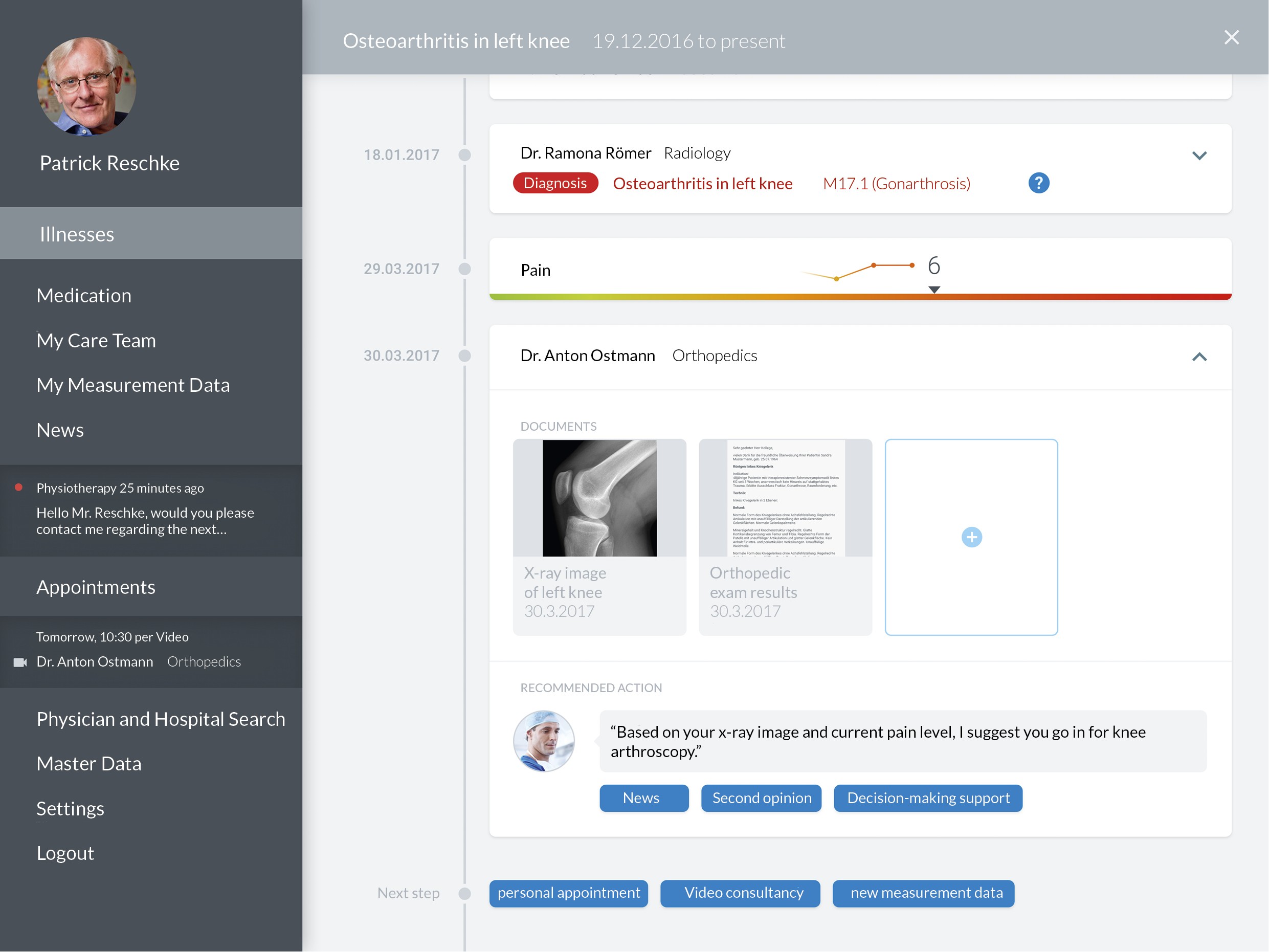
The basic conceptual idea is of particular importance to us, and we will continue to work on this together with Peter Haas in future. Electronic health records aren’t “just” an instrument for the cooperation of service providers – they are the technological lever for active cooperation of patients and treatment providers, and, not least, can effectively support self-management. Moreover, they aren’t “only” an interactive storage and management location for data – they are the foundation for the comprehensive treatment management of patients. In this scenario – and this is the overarching concept – electronic health records form the central instrumental foundation for the digital transformation (of communication) in the healthcare sector – a kind of “hub” for digital process innovation.
In future, a wide array of digital processes could be represented on these treatment management platforms – whether an original product of a record system, or by means of intelligent interfaces. To name just a few examples, the record could be a platform for:
- tele-consultation between physicians,
- saving and observing the data from remote patient Monitoring,
- digital communication between patients and service providers, for example, in the form of video consultations,
- enabling patients to obtain a second opinion,
- the management of self-reported data, or
- the sharing of evidence-based health Information.
The latter, in particular, makes it clear why the electronic patient record is so suitable as a platform: Here, where all information on the health condition of a patient flows together and the ongoing treatment process is planned, is where the need for information arises. In the record, patients could call up evidence-based information in a context-sensitive manner, without a “detour” of search engine research. For example: A physician gives a treatment recommendation based on a diagnosis in the record. Ideally, the patient can translate the diagnosis directly into language comprehensible to the layperson, and display explanatory health information or a decision-making tool. The patient can then discuss this with their physician, for example, in a video consultation.
It is clear that in this scenario, access to the record for the patient has to be more than simply a “patient file” from which documents can be accessed and their own documents edited. It is also evident that the implementation of these kinds of platforms is far from a trivial exercise, and that there are many questions to be answered and decisions to be made: On the content, data protection, access management, interoperability standards, accepted operator models, and, not least, on financing. Another point of discussion is how those that cannot (or do not want to) control or moderate the content themselves can profit from the advantages of electronic health records. All of these issues will not be resolved overnight – implementation can, and should, take place incrementally.
However, we think it is worthwhile and of critical importance to pursue the mission of comprehensive treatment management platforms from the very outset. We think that now is the time to discuss which steps need to be taken to get there, what frameworks need to be established, and, for example, which governance model is appropriate for the implementation process (the discourse on this began right after the expert report was published). With this in mind, we regard the expert report by Peter Haas as catalyst for discussion, and look forward to further exchange on the issue; also in this blog.
This blog post is the kickoff for a series of posts on the topic of electronic health records. In these posts, which will be published at irregular intervals, we will address individual issues analyzed in the expert report by Peter Haas, and also let other stakeholders have their say.
Related links:
- Download SPOTLIGHT Healthcare
- Download Expertise (available in German only)
Click here to subscribe to our newsletter:

