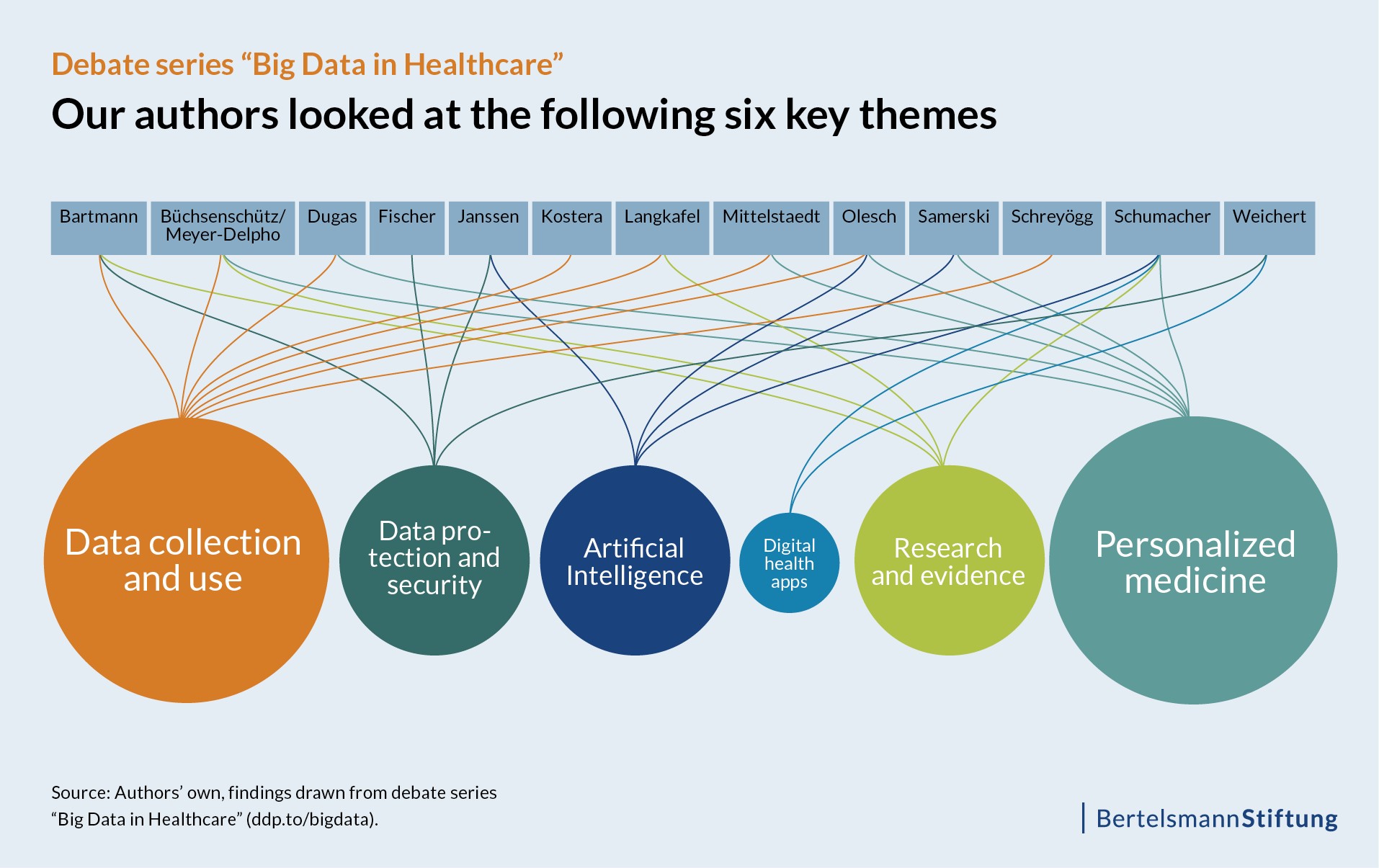
In a debate series held in the past several months, the Digital Patient project has focused on the opportunities and challenges presented by big data in the healthcare sector. Our blog became a platform for a range of experts to have their say on the issue. In this post, we analyze the 13 contributions to the debate series and summarize the results.
In our debate series, a variety of science, healthcare, business and media experts explored a different facet of big data in healthcare. We evaluated their contributions systematically, and now it’s time to take a look at what they see ahead – big data’s opportunities and challenges, the available solutions and where, exactly, the future of big data lies in the healthcare sector.
Big data has the potential to individualize treatment and optimize research
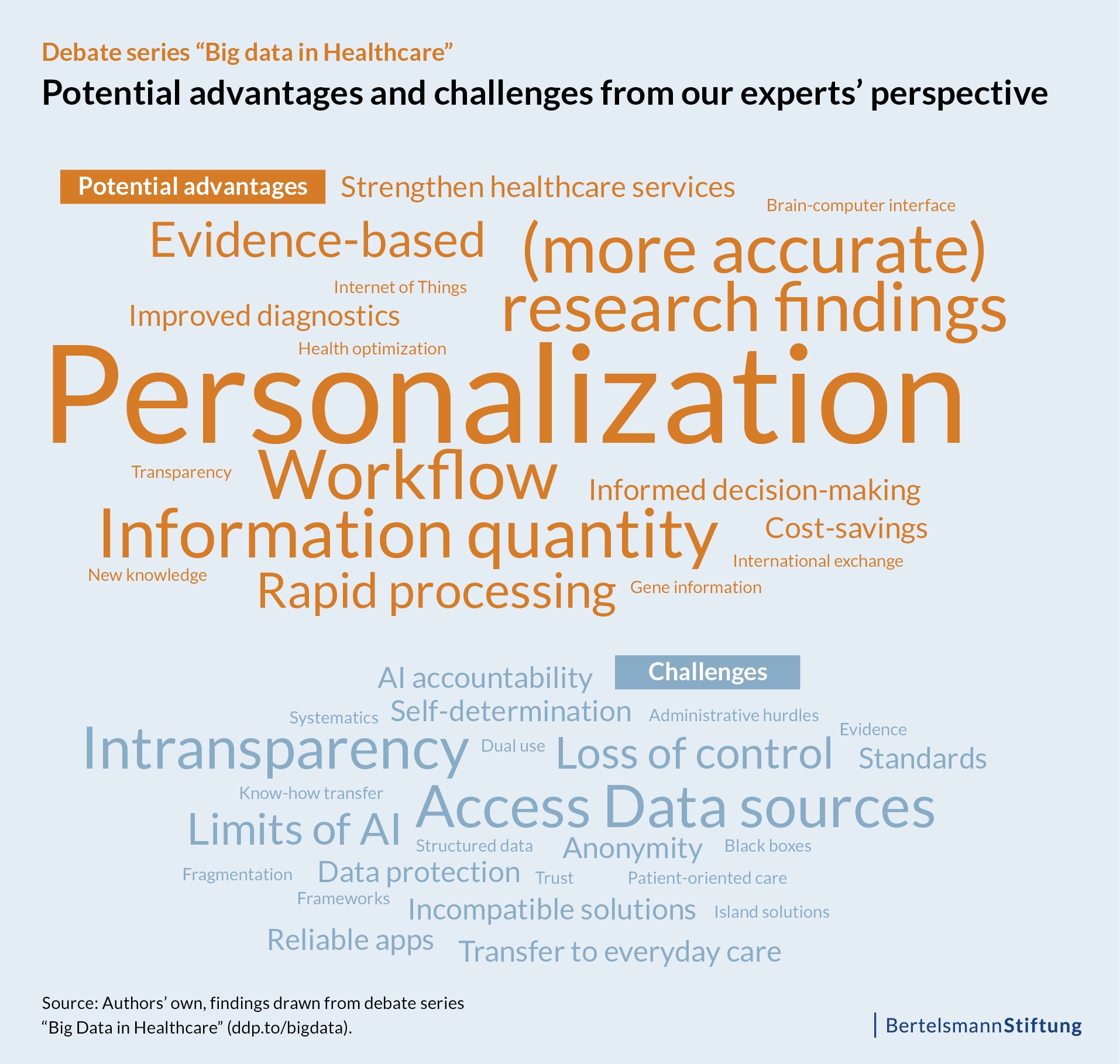
Big data holds tremendous potential in personalizing diagnoses, treatments and medications. This conclusion is shared by most of the experts who contributed posts. Many of the authors also identified the fast pace of diagnoses and data analysis made possible by algorithms and artificial intelligence as one of big data’s advantages.
Another potential benefit identified by several authors is the fact that the analysis of large amounts of data makes it possible to better substantiate diagnoses. The authors see big data as an opportunity to achieve more accurate research findings for use in evidence-based medicine. This newly generated evidence, in particular, holds the greatest potential for improving care.
The challenge: We need a more systematic handling of big data
However, alongside these major advantages, the experts also point to significant challenges. Al of our authors agree that data access and processing pose the largest hurdles. As they note, much of the data is unusable – because the data is completely unstructured, not easily acquired or simply not accessible at all. In addition, they note that there are no standards regulating data collection and use. It appears that there are also problems in the structure of the healthcare sector itself; some of the authors emphasize the sheer lack of connectedness, which results in a myriad of isolated and incompatible solutions, for example different software tools that each have their own forms of documentation forms.
Our authors, or at least those experts who focused on the subject of artificial intelligence (AI), view it critically. Although it can be of help to physicians in making a diagnosis and selecting the appropriate treatment, AI is seen as being quite problematic. This is because, as the experts note, AI processes influence decisions in ways that are often difficult for patients to verify or understand.
While ethical questions are the focus how to handle AI processes, in the field of digital health applications, such as health apps, our experts place the focus on questions of quality, pointing out that some tests are unreliable while others fail to sufficiently maintain anonymity and give users too little control over their personal Information.
Improved classification and increased responsibility will harness big data’s potential
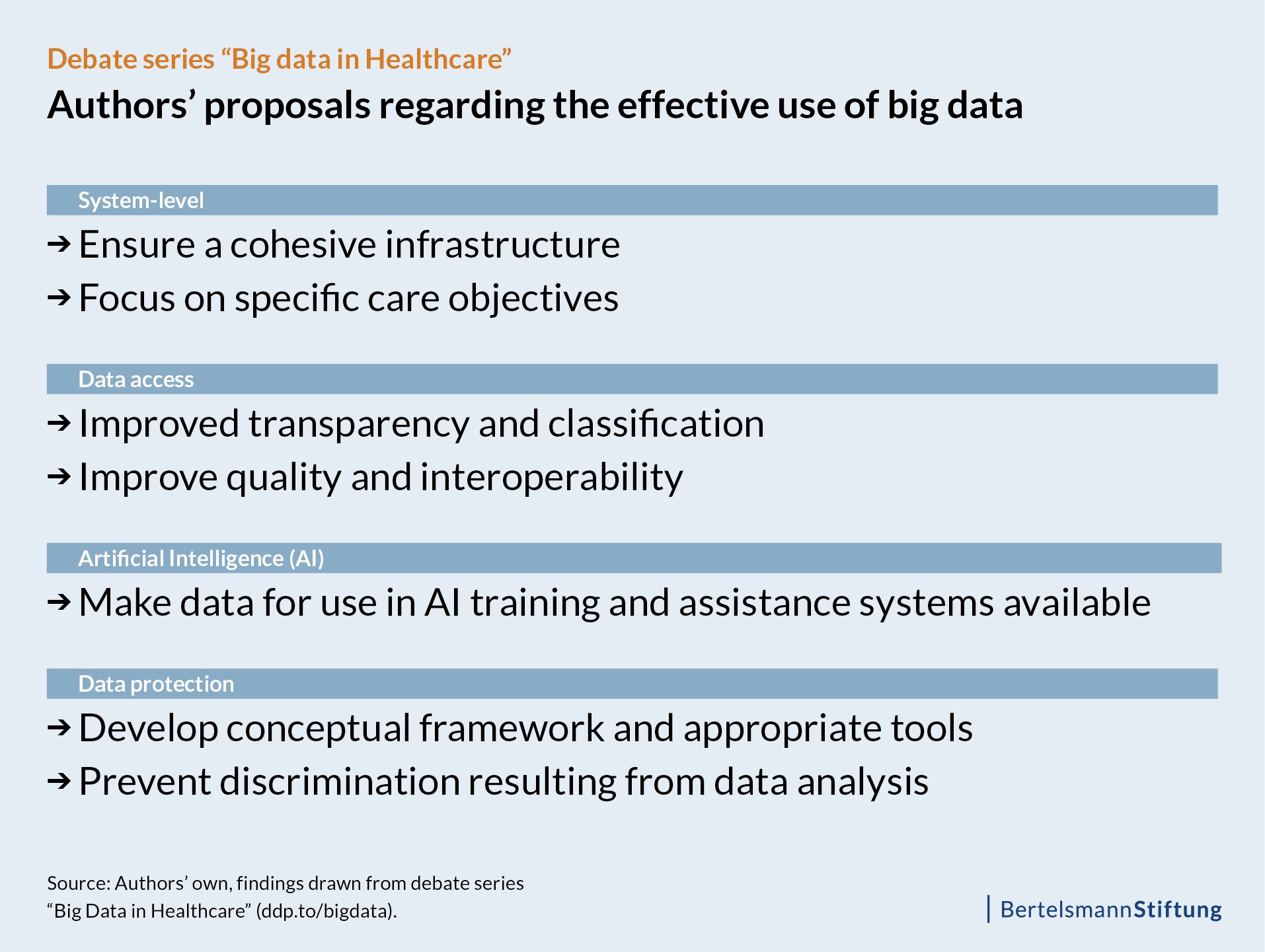
Each author specified different demands and solutions for the future depending on the focus of their article. However, they all suggested that actors in politics, business, research and healthcare should take a more systematic, constructive and goal-oriented approach to big data while, at the same time, maintaining full awareness of accountability.
With regard to accessing and processing data, our analysis also shows that for the experts, the way forward in handling big data involves publishing structural, performance and SHI routine data, improving data quality and deepening transparency.
The authors examining AI argued that it should be used to a greater degree in the future so as to render this data usable. However, they also noted that AI should serve primarily to assist human decision-making and that responsibility for decisions should always lie with physicians and care professionals.
Data protection was also a key theme. In order to increase data protection for patients, our experts proposed using encryption and anonymization tools as well as trustee models. The idea would be to familiarize patients with the processes and provide them with understandable and sufficient information as to who exactly collects data and for what purpose – all in an effort to strengthen patient autonomy. Indeed, the authors see a significant need for action in the future, especially with regard to data sovereignty and the handling of artificial intelligence.
A glimpse into the future of data usage and artificial intelligence
The authors who offered predictions in their contributions see the Internet of Things (IoT) as a key catalyst for big data in the not-too-distant future. Other important future themes are artificial intelligence and its influence on healthcare, as well as the role of physicians.
With regard to artificial intelligence in particular, our experts noted that a number of questions remain open. In the future, AI will increasingly serve to assist physicians and care staff in their work. Thanks to data analysis, AI will also underlie decision-making in the provision of care. For this reason, the authors posed the question as to how – and to what extent –complex decision-making workflows among physicians could be automated. Another question that drew their attention was whether physicians will increasingly come under pressure if they choose to differ with what the computer is telling them, or if they are simply not what one might call “computer oriented.”
Click here for an overview of all 13 articles in the “Big Data in the Healthcare Sector” debate series (in German). The findings of this series will form the basis of our exploration of big data issues in the Digital Patient Project.
Click here to subscribe to our newsletter:

